Glioblastoma (GBM), the most common primary brain tumor, represents one of the most aggressive cancers. The signaling from PI3K and AKT to mTOR is commonly dysregulated in GBM. But, blockade of these upstream targets minimally affects mTOR activity in glioma. Allosteric mTOR inhibitors, such as rapamycin, incompletely block mTORC1 compared with mTOR kinase inhibitors (TORKi). in this study, RapaLink-1, the third-generation bivalent mTOR inhibitor, combines Rapamycin with MLN0128 (a second-generation mTOR kinase inhibitor) by an inert chemical linker. RapaLink-1 shows better efficacy than Rapamycin or mTOR kinase inhibitors (TORKi), potently blocking cancer-derived, activating mutants of mTOR. It can cross the blood-brain barrier. RapaLink-1 binding to FKBP12 results in targeted and durable inhibition of mTORC1. It also plays an antithrombotic role in antiphospholipid syndrome by improving autophagy.
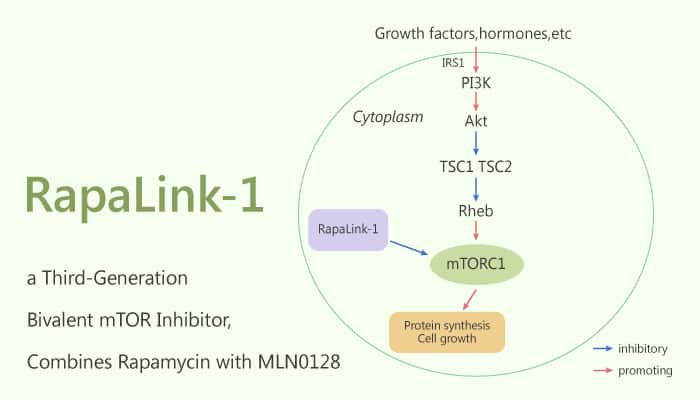
mTOR is a central therapeutic target in GBM. Rapalink-1 is more potent than first- and second-generation mTOR inhibitors, with no significant toxicities. RapaLink-1shows U87MG cells growth inhibition and arrests of U87MG cells at G0/G1. RapaLink-1 selectively inhibits p-RPS6S235/236 and p-4EBP1T37/46 at doses as low as 1.56 nM. Moreover, it exploits the unique juxtaposition of two drug-binding pockets to create a bivalent interaction. RapaLink-1 overcomes resistance to existing first- and second-generation inhibitors. In addition, RapaLink-1 shows potent anti-tumor efficacy.
In summary, RapaLink-1 is a TORKi linked to rapamycin, with earlier-generation mTOR inhibitors. RapaLink-1 associated with FKBP12, an abundant mTOR-interacting protein, enabling the accumulation of RapaLink-1. RapaLink-1 showed better efficacy than rapamycin or TORKi, potently blocking cancer-derived, activating mutants of mTOR. In addition, it can cross the blood-brain barrier and could induce regression in the orthotopic xenograft, PDX, and genetically engineered models for brain cancer. This class of agents thus holds promise for future therapy of patients with GBM.
Reference:
Fan Q, et al. Cancer Cell. 2017 Mar 13;31(3):424-435.