BMI-1 is a highly conserved class II member of the Polycomb group of genes, regulating diverse aspects of transcription, stem cell maintenance, cell proliferation, and oncogenesis. BMI-1 has vital functions in the self-renewal and maintenance of AML and normal hematopoietic stem cells.
The first BMI inhibitor PCT-209 has a positive effect in numbers of cancers; it can potently inhibit tumor cell growth and eradicates cancer-initiating cells.
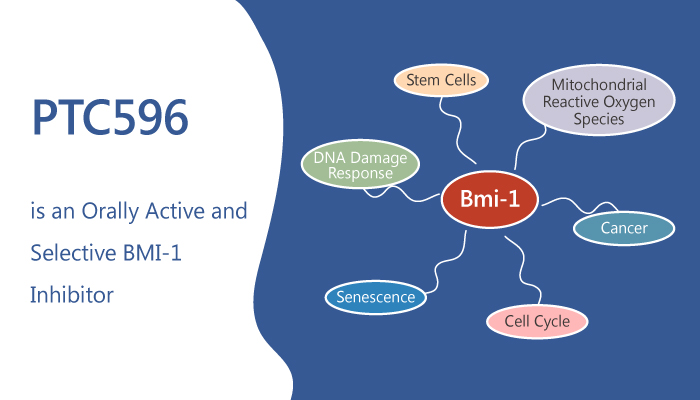
Today, we will introduce another small molecular BMI-1 inhibitor, PTC596; it is an orally active and selective BMI-1 inhibitor with a favorable safety profile.
Firstly, in vitro, the authors choose several AML cell lines to examine the PTC596 effect on its viability. PTC596 inhibits AML cell line growth with mean average IC50 and ED50 of 30.7 nm and 60.3 nm, respectively. Besides, PCT594 induces cell apoptosis in a p53-independent manner in AML cells.
Secondly, PTC596 can reduce anti-apoptotic MCL-1 protein expression through post-transcriptional protein synthesis inhibition in AML cells. Moreover, PTC596 can trigger mitochondrial apoptosis by destabilizing the mitochondrial membrane, changing BAX conformational, promoting caspase-3 cleavage, and phosphatidylserine externalization.
Lastly, the authors prove the importance of PTC596 by several mouse models. PTC596 can lead to a significant reduction of circulating human CD45-positive cells in the blood in the highly aggressive MOLM-13 xenograft model. PTC596 reduces the mean tumor volume of mice by comparing it with control mice in the K562-bearing mice. Besides, PTC596 improves the anti-leukemic activity in HL-60 xenograft mice, in which PTC596 significantly prolonged mouse survival in a dose-dependent manner.
In summary, PTC596, as a promising BMI-1 inhibitor, it can decrease MCL-1 expression and induce mitochondrial apoptosis in a p53-independent manner in vitro. Meanwhile, PTC596 can prolong mouse survival by improving anti-leukemic activity in vivo. These findings strongly encourage the development of BMI-1-targeted therapy for AML patients.
Reference:
Nishida Y, et al. Blood Cancer J. 2017 Feb 17;7(2):e527.